How To Become A Vascular Access Nurse?
Did you know that certain nurses can choose to specialize in giving intravenous infusions, a talent you may have noticed when you’ve had one yourself or seen a patient on a medical drama grimace through one?
Vascular access nurses have the knowledge and skills to make procedures like these more complex ones as comfortable as possible for their patients. Simply put, what does the term “vascular access nursing” mean? In what ways are these nurses trained? Please read on to find out more about this challenging area of nursing.
Needles and IVs are two things that most of us associate with unpleasant medical experiences. You can only imagine the impact a well-trained nurse can have if you’ve been poked multiple times in one visit or if your nurse did the job with just one stick.
What are Vascular Access Nurses?
As the name suggests, vascular access nurses specialize in the procedures and knowledge required to gain access to a patient’s veins. That may be more challenging than it seems. These registered nurses introduce peripherally inserted central catheters (PICCs) and central venous catheters (CVCs), two of the most complex types of intravenous lines (CVCs).
If a patient needs to leave the facility with a vascular access line, the nurse will instruct them on keeping clean and free of infection after returning home.
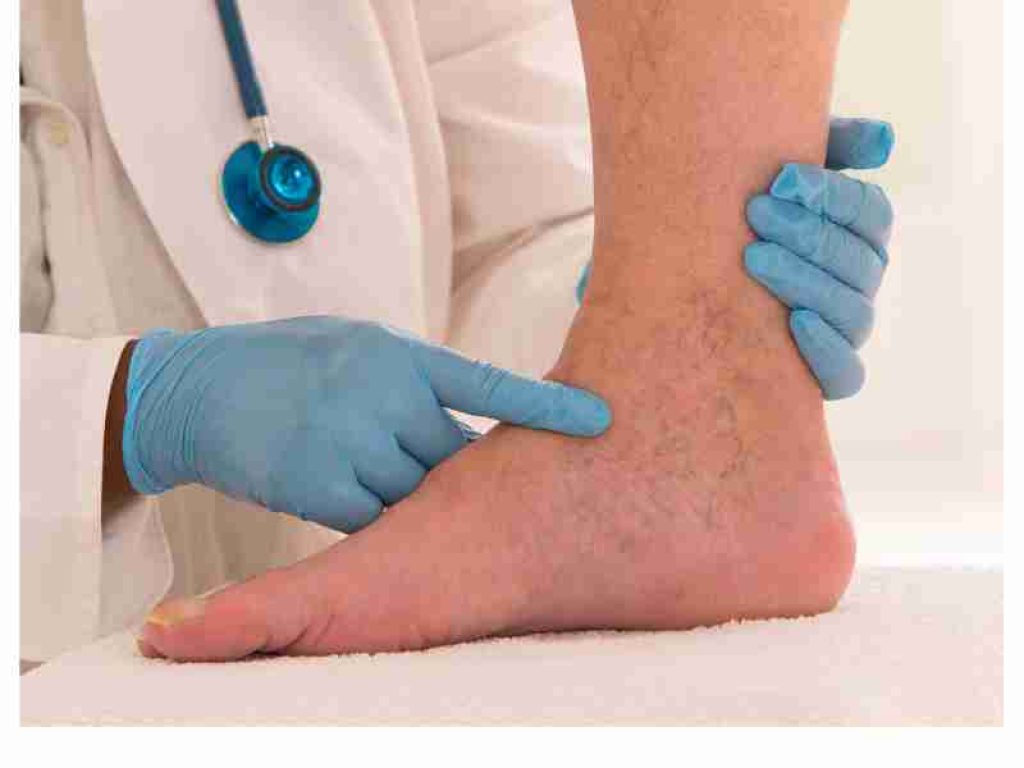
Vascular access nurses work closely with doctors, deciding what kind of line to carry out these duties. To double-check the line’s location, they may coordinate with radiology. Plus, when placing lines, they must speak with patients. Typically, these nurses work in healthcare settings like hospitals, clinics, and nursing home wards.
Although vascular access and IV/infusion nurses share some responsibilities, the latter is limited to administering nurses or infusions through the patient’s IV or other vascular access port. At the same time, the former is responsible for setting up the line.
What are the certification requirements for vascular access nursing?
A vascular access nurse must have a minimum of a two-year nursing degree, preferably a Bachelor of Science in Nursing (BSN) or an Associate of Science in Nursing (ASN) (ADN). Despite their variations, both programs will put you in a good position to enter the nursing nurse and earn your RN license (RN).
Certified Registered Nurse in Infusion (CRNI®) or Vascular Access Board Certification (VA-BC®) certificates are two examples of valuable professional certifications that can help you stand out and demonstrate your dedication to this field. Though these may be only suggestions or preferences for some positions, they may be necessary prerequisites for others.
Experience with IVs and other forms of vascular access is valuable in addition to qualifications in this field. You can learn and gain valuable experience in this area through clinical rotations in a nursing school. Work as a phlebotomist or in intensive care, oncology, or emergency room, where IVs, PICC lines, and CVCs are often used, to add non-clinical experience to your resume.
What duties do Vascular Access Nurses fulfill?
One type of registered nurse, the “vascular access nurse,” focuses only on the needs of patients who have central venous catheters (CVCs). They are in charge of managing any difficulties that result from CVC placement, maintenance, and removal.
Vascular access nurses collaborate with doctors and the healthcare staff to deliver the highest standard of care for every individual patient.
The duties of a vascular access nurse include the following:
- Putting in patients’ central venous catheters (CVCs)
- Keeping a close eye on patients in case of CVC-related issues
- Giving patients and their loved ones information about how to care for a central venous catheter
- Disposing of CVCs when their use has expired
- Keeping detailed logs of all medical procedures
- Individualized treatment plans are developed in collaboration with various healthcare team members.
- Acting as a supervisor for more junior employees
How to become a Vascular Access Nurse?
If you want to work as a nurse in vascular access, you need to follow these guidelines.
Getting an Associate’s or Bachelor in Nursing:
To enter the field, one must complete an associate’s or bachelor’s degree program in nursing. Although a BSN is often required for a position as a vascular access nurse, some employers may be willing to consider candidates with an ADN (ADN).
To obtain an undergraduate degree in healthcare, you must generally complete two to four years of study that involves anatomy, physiology, pharmacology, nutrition, ethics, and patient care. Through clinical rotations, students can gain hands-on experience working with patients and nurses in a supervised environment.
Pass the National Council Licensure Examination for Vascular Access Nurses (NCLEX-RN):
To become a vascular access nurse in the United States, you must complete nursing school and pass the National Council Licensure Examination for Registered Nurses (NCLEX-RN) (RN).
You will be tested on your knowledge and skills on the NCLEX-RN through multiple-choice questions. You must achieve at least 75 on each test section to pass.
First, you’ll be quizzed on your medical know-how and then on your nursing chops. If you don’t pass the first time, you’ll have another chance to do so once a specific period has passed.
Gain practical experience in a medical setting:
After finishing your education, you’ll be qualified to apply for vascular access nurse jobs. Before going down this road, you should get experience working at a hospital. There is a need for nurses with experience in vascular access who can work long shifts and be on call.
You could further your career in vascular access nursing by pursuing extra education and certification. Healthcare providers and institutions frequently provide such courses.
nursing license from the American Nurses Credentialing Center (ANCC):
The organization grants certification in the specialty to vascular access nurses who have fulfilled the ANCC’s qualifications. A valid RN license, one year of vascular access experience, and passing a multiple-choice exam are all prerequisites for the ANCC vascular access certification.
Nurses who have earned the ANCC’s certification in vascular access may use it to move up the ranks, either by taking on leadership roles or becoming educators in the field.
Improve your ability to communicate with others and express yourself clearly:
Caring communication skills are essential for nurses working in the field of vascular access. They need to be able to interact effectively with other medical professionals. Listening skills are essential for nurses to address patients’ worries.
Keep abreast of developments in the medical field:
Even though vascular access nursing has been around for a while, it has evolved alongside the rest of the medical field. Nurses specializing in vascular access must remain current on the latest findings and methods in their field to give optimal patient care. Introducing novel techniques or technologies may necessitate the education of vascular access nurses.
Additionally, vascular access nurses need to be aware of the frequent changes in the legislation and laws that regulate vascular access nursing.
The American Nurses Association (ANA) is a great organization for you to join:
Vascular access nurses can find help and further their knowledge through the American Nurses Association (ANA). The Association of Vascular Access Nurses (ANA) provides its members with chances to further their education, remain abreast of relevant medical discoveries, and establish professional connections. The American Nurses Association (ANA) is a great resource for anyone seeking a career in vascular access nursing.
What is the Salary and Job Prospects for Vascular Access Nurses?
Vascular access nurses earn a median annual salary of $87,550. Salary ranges for registered nurses can differ widely depending on factors such as their years of experience, degree of education, nurse, and region.
According to the BLS, the job market for registered nurses with expertise in vascular access should grow at a faster-than-average rate over the next decade. This is because of the rise in chronic illnesses that necessitate vascular access as the population ages.
Which difficulties are associated with vascular access nursing?
Working with needles and blood is an evident requirement of this career. If you are queasy about blood or needles, this is not the right specialty for you.
Many patients feel the same way, which is why the top vascular access nurses can put their patients at ease. Possessing a soothing, compassionate personality and an optimistic outlook is essential for this work, whether speaking with a patient to divert them or waiting for the patient to relax.
Finally, vascular access nurses are often called upon to help patients with significant hurdles, making it exceptionally difficult to get a lineup successfully. It is very uncommon for a patient to experience some discomfort due to the multiple attempts required to locate and access a vein.
Sometimes, even the most skilled vascular access nurses must make it a few times before they get it right. The trick is to show compassion for the patient while getting the work done quickly and with minimal damage.
However, this specialist position is only in some facilities, which presents an additional challenge outside direct patient care. While there are always exceptions, vascular access experts are often exclusively maintained in major hospitals and health systems due to the high cost and constant patient demand.
How does one describe the positive aspects of working in vascular access nursing?
Despite the needles, vascular access nursing can be very satisfying if you enjoy helping people. Working directly with patients allows you to see the life-changing effects of your treatments. You get to see the improvements in patients, from increased mobility to a final check-out at home.
The hands-on nature of this position extends to teaching patients how to maintain their lines in the comfort of their homes. This could be your dream job if you enjoy sharing your knowledge with others. Any patient would be grateful to have a nurse who could relate to their apprehension about injections. Patients are appreciative if you can calm their nerves with just one poke or a few words the first time you see them.
Additionally, lending aid to other nursing departments with difficult cases can be rewarding when you draw blood on the first attempt or successfully place a line. Doing work that calls for expert-level knowledge and training flawlessly is a source of great satisfaction.
Does a job in vascular access nursing good for you?
Knowing what you know now about vascular access nursing, you can appreciate the significance of this field and the positive impact a skilled practitioner can have on the quality of a patient’s life.
Even if doing this work makes you queasy, you should give it a shot. Some people aren’t cut out to work in an environment where they constantly deal with sharp objects, tubes, and wires. While there may be a better nursing specialty for you, there are dozens of others.
Conclusion
Vascular access nursing is a challenging yet rewarding field of nursing. It requires a compassionate personality, an optimistic outlook, and the ability to remain calm under pressure. It also requires specialized knowledge and training to be able to place lines and draw blood on the first attempt successfully. Working in this field can be very satisfying as you get to see the life-changing effects of your treatments and help patients maintain their lines in the comfort of their homes. If you think this job is right for you, then give it a shot!